The CDC just approved vaccines from Americans aged 5-11. That’s great news! But today, I want to talk about another age group: mine.
A few months ago I wrote a post summarizing data for COVID-19 deaths among people in their 30s and 40s. While we have primarily thought of COVID as a disease impacting the elderly (and indeed in the aggregate, it is), there have been major health consequences for those under 65 too. Including major health consequences for the age group 30-49 (which I believe is the age range of all our bloggers here at EWED).
I wanted to update that data because a few new things have come to light. First, I highly recommend reading a recent paper by my friend Julian Reif and co-authors. They estimate the number of Years of Life Lost and Quality-Adjusted Years of Life Lost for different age groups from COVID-19. Their data runs through mid-March 2021, so before vaccines probably had much of a chance to impact the aggregate death numbers (though vaccines were being rolled out at the time).
Here’s their main result: while most of the deaths from COVID were among those aged 65 and older (80% through March 2021), most of the life lost in terms of years was for Americans under 65 (54% of QALYs). And even for very young adults, the risk in terms of years of life lost was not minimal. A comparison from the paper: “Adults aged 85 years or older faced 70 times more excess risk for death than those aged 25 to 34 years but only 3.9 times more individualized loss of QALYs per capita.” Compared to the 35-44 age group, the relevant factor is 2.8 times more individualized loss for the 85+ group.
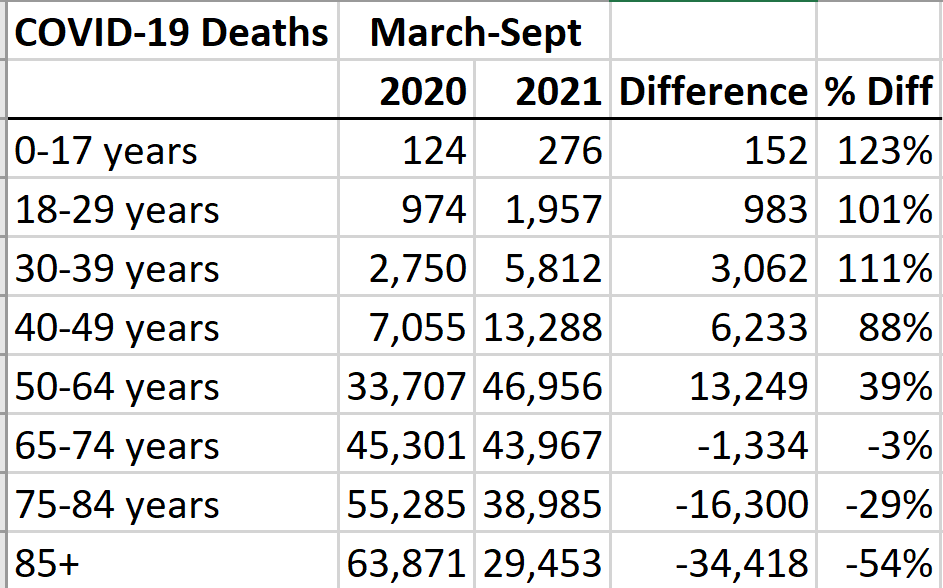
It’s a great paper, but it only goes through March. What has happened since March 2021? While 80% of the COVID deaths up through March 2021 were among the elderly (65 and older), since April 2021 only 60% of the COVID deaths have been among the elderly. Part of this is because deaths are down among the elderly, but it’s also because deaths are up for the non-elderly. The table is my attempt to show this effect, looking at the period from March-September in both 2020 and 2021 (data is current as of October 27, so the September 2021 data is still not complete, but instructive).
For the oldest Americans, COVID deaths fell by 50%. That’s great! But for younger Americans, COVID deaths roughly doubled. Not good!
Continue reading